LISTEN TO THIS ARTICLE:
Every 11 seconds
Approximately 800,000 people die from suicide around the world each year. In the United States, someone dies by suicide every 11 seconds. Not only are adults struggling, suicide rates among children and teenagers are also rising. It is the second most common cause of death in this population. The strongest predictor of a future suicide attempt is a previous suicide attempt. With this knowledge, the mental health field has shifted the focus of suicide research toward more practical, concrete, and immediate interventions. One effective intervention is the Stanley-Brown Safety Plan.
This type of safety plan was developed by Dr. Barbara Stanley and Dr. Gregory Brown, two experts in the field of psychiatry, with the intent of preventing repeat suicide attempts. For years, mental health professionals had their clients sign a “no-suicide contract.” This was a document a person signed where they promised not to harm themselves. However, there was little evidence that this intervention helped those struggling. Dr. Stanley and Dr. Brown recognized the need for a more beneficial tool that involved a person’s active participation in the planning process.
How the safety planning intervention works
The first goal of safety planning is to become more aware of personal warning signs that signal a suicidal crisis is beginning or growing.
Safety planning aims to develop self awareness. The first goal of safety planning is to become more aware of personal warning signs that signal a suicidal crisis is beginning or growing. The second goal of safety planning is to have coping strategies, sources of distraction, and resources available to the person in distress. However, the unique part about the Stanley-Brown Safety Plan is that the person at risk writes their own plan in collaboration with a mental health professional. The plan is brief and can be used immediately during moments of crisis. It is a hard copy of a document that can be kept on a person at all times so that it is always available.
Risk and time
The Stanley–Brown Safety Planning Intervention is based on a risk and time curve. The image below shows how a person’s level of suicidal risk can increase or decrease over time.
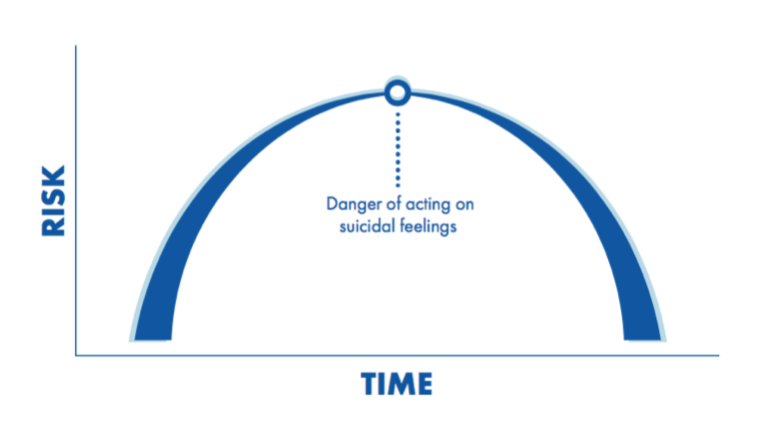
As warning signs increase over time, risk also increases. The most dangerous moment for a person is when they reach the top of the curve. Here, they are at highest risk of acting on their suicidal thoughts. This stage is known as acute suicide risk. The goal of the Stanley-Brown Safety Plan is to prevent a person from reaching this point through recognizing their own warning signs. If a person does reach the top of the curve, they already have a written plan created to help them. Safety planning includes identifying effective coping strategies that will help a person through this difficult period of time. Using coping strategies decreases their level of suicide risk and helps them move past the acute risk period.
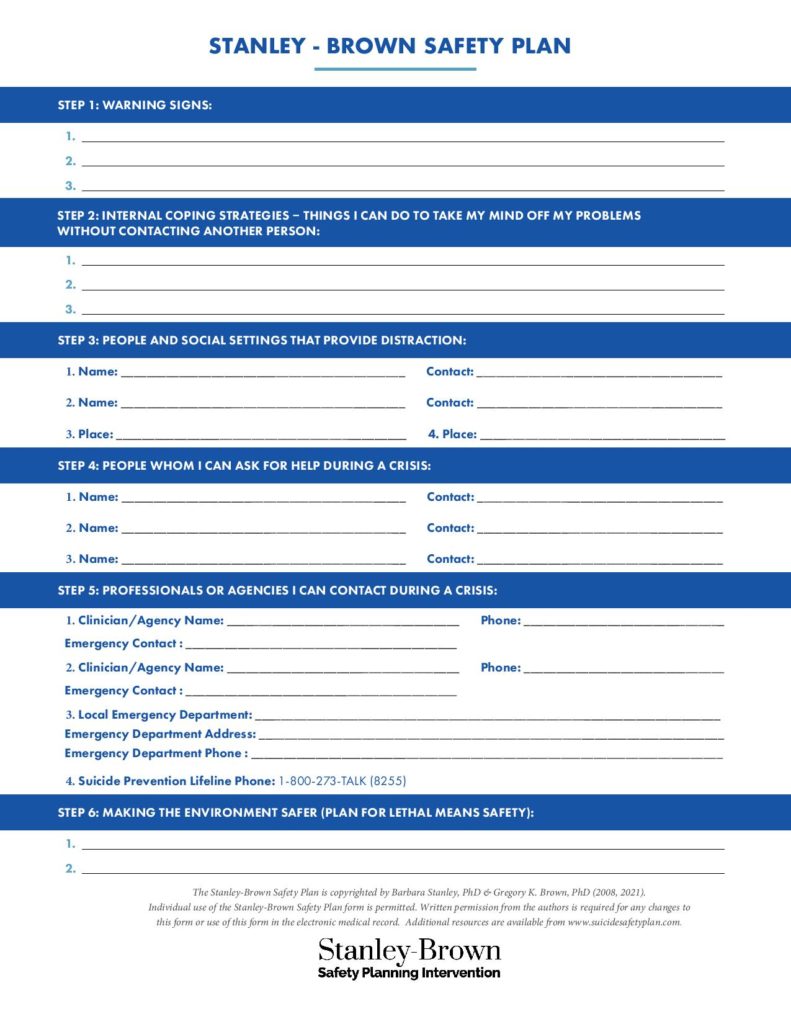
The Six Steps of the Stanley-Brown Suicide Safety Plan Intervention
1. Identify warning signs
The first step of the safety plan asks a person at risk of suicide to identify their own personal warning signs. A mental health professional may ask a patient to tell the story of their first suicide attempt. Together, they talk about what the warning signs were and write them down on the safety plan. Examples of warning signs include feeling like a burden to others, changes in eating or sleeping habits, isolating from others, and feeling empty or hopeless. Remember that every person’s warning signs will be unique and different.
2. Implement internal coping strategies
The second step of the safety plan is creating a list of internal coping strategies that a person can use to distract themselves in a time of crisis. Having the ability to distract themselves through positive and enjoyable activities is important until they can seek support from others. Activities include exercising, reading a book, or completing a home improvement project. This is a critical initial step. Often, people are alone when they are struggling.
3. Distraction through social situations
If step 2 is not enough to distract a person from suicidal thoughts, the next step has a person surround themself with other people. During this step, they will not yet disclose their feelings to others. Instead, they attempt to distract themself through positive interactions with those around them.
4. Ask for help
If a person is unable to distract themselves in steps 2 and 3, step 4 involves developing a list of people they feel comfortable going to asking for help. This list includes anyone that the person trusts and will confide in when struggling.
5. Contact professionals or agencies
Step 5 encourages a person to contact a professional or agency if needed. Examples of agencies include the National Suicide Prevention Lifeline (call or text 988), the American Foundation for Suicide Prevention, and the Suicide Prevention Resource Center. The National Suicide Prevention Lifeline offers 24/7 support for those in immediate need. The service is free and confidential.
6. Make the environment safer
The last step of the safety plan includes restricting access to lethal means. In order to make the environment safer, the clinician will work with the client to think about any dangerous items the person at risk may have at home. This can include old medication prescriptions or firearms.
Benefits of the Stanley-Brown Safety Plan
Emergency departments are often the fist place a person with acute suicide risk will go for treatment. The benefits of the Stanley-Brown Safety Planning Intervention has been well researched in emergency mental healthcare settings. A 2018 study included 1,640 patients at Veterans Affairs hospitals in the United States who were admitted to an emergency department for acute suicide risk. The researchers reported that a written safety plan with follow-up phone calls reduced suicidal actions by 45 percent.
A written safety plan with follow-up phone calls reduced suicidal actions by 45 percent.
The period after visiting the emergency department is a high risk period for suicide. This is a critical time where continued mental health treatment is very important. However, many people do not receive the help that they need. Using a safety plan and follow-up support, the patients in the study were two times more likely to seek treatment during the six months after their initial visit to the emergency department. With suicides rising, these safety plans could be a critical tool in saving lives.


 Learn
Learn Read Stories
Read Stories Get News
Get News Find Help
Find Help
 Share
Share
 Share
Share
 Share
Share
 Share
Share



