LISTEN TO THIS ARTICLE:
This is the first of a two-part series on dementia and cognitive decline. In the second part, we explore what friends and family can do to help a loved one with the disease. Read Part Two here >
Seeing Through Their Eyes
“Who is that? She’s bringing me food. That’s nice. She looks familiar…I can’t think of her name.” It’s hard to imagine forgetting what to call your spouse, children, or friends you have known for decades. All that information seems so permanent in our minds – until it isn’t. Dementia is a devastating process that slowly destroys a person’s ability to form and retrieve memories.
Alzheimer’s Disease is the most common form of dementia, and represents up to 80% of cases. As the illness progresses, it steals more and more skills: making communication harder, causing movement issues, and changing moods. By the end, sufferers need round-the-clock care. They can no longer form intelligible words and are largely bed-bound.
It is a tragic end to a devastating illness. This state is what most people imagine when they think of dementia. It carries a stigma, an assumption that sufferers are helpless. But people can live up to 20 years after the initial diagnosis. There is plenty of time to enjoy life before the very end. The best way that friends, family, and treatment providers can help is by trying to understand what people are experiencing at different stages of their illness.
Setting the Stages
Depending on who you ask, you’ll find sources claiming that dementia has at least three and sometimes up to six or seven separate stages. The truth is that dementia is a spectrum, a gradual decline rather than a series of discrete steps. We break it into stages to make it easier to understand, describe, and treat, but that’s not really the experience.
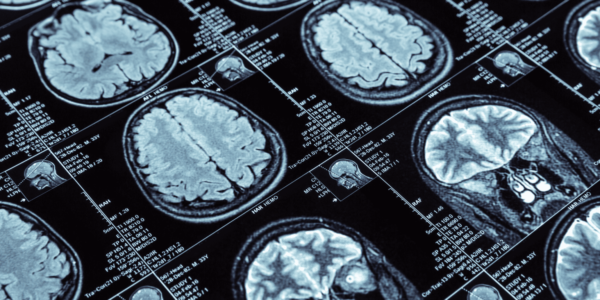
The earliest stage begins when the first brain changes begin – years before any noticeable symptoms appear. Medical imaging reveals amyloid (a protein that impairs signaling in the brain) deposits starting to build up. Although some studies have discovered mild decreases in attention at this stage, most people will not notice anything serious. They continue to live their lives without interruption or difficulty. They work, vacation, and enjoy the company of friends and loved ones. Their lives are unchanged – so far.
Getting Harder to Ignore
“You told me that story already, Dad.” “You didn’t go to your meeting?” “You forgot your doctor’s appointment?” This is a taste of early cognitive decline. People start to forget recent conversations they have had and details about new people they have met. They miss meetings and have trouble focusing on tasks.
Taken individually, instances like this sound entirely within the realm of normal. We all miss things from time to time. Why worry about it? This is a reasonable response, and many people dismiss, deny, or explain away their initial symptoms. However, as forgetfulness progresses, it becomes harder to believe it’s just a few isolated instances. Family members, friends, and work associates start to see the pattern grow until it becomes undeniable.
The disease may make them seem foreign and absent, but they are absolutely still alive…To the very end, people with dementia…benefit from having company and genuine human companionship…having someone caring nearby helps give them peace.
Mild Cognitive Impairment
The first visit to the doctor often brings up the question: Is this the dreaded dementia or the much less terrifying Mild Cognitive Impairment (MCI)? While many may not have heard of MCI, it is pretty common, appearing in 15-20% of people over age 65. People with MCI have vague memory deficiencies and other thinking issues, such as trouble with problem-solving, losing items, and word-finding difficulties. At this stage, people can still work and lead independent lives. They use reminders like taking notes and using calendars to compensate for cognitive losses. Symptoms like this are often – but not always – a prelude to the progressive deterioration of dementia.
About 80% of people with MCI go on to develop dementia within seven years. Only 1-3% of people in the same age group develop dementia without first having MCI. Though it’s difficult to tell who will go on to get worse, generally, those with more severe MCI symptoms are more likely to develop dementia eventually.
Downward Slide
When symptoms of this early period progress beyond mild memory impairments, dementia has reared its head. People start having trouble with ‘big-picture thinking.’ They have trouble planning, managing their finances, and solving complex problems. Finding the right words to express themselves gets harder and causes frequent frustration. Activities of everyday life take a little more effort and time. Even leaving the house gets more challenging, as people may forget where they are, where they are going, or what day it is.
At this stage, many can still compensate to some degree. They may continue to live independently, and those they don’t know probably won’t notice any issues. However, family, friends, and doctors will most definitely notice.
Processing the News
For most, receiving a diagnosis of dementia is earth-shattering. Some may react with anger, thinking, ‘How could this happen to me? This is not how I saw my life going. I’ve always been healthy, so why this now?’ Fear and uncertainty about the future are a given. Loneliness is common, as are anxiety and depression. The sole positive (if you can call it that) for some is the ability to finally give a name to the growing symptoms they are experiencing.
Newly diagnosed and thrust into a sea of confusing and painful emotions, it is easy to miss a significant opportunity here. At this stage, most people are still capable of making major life decisions. People can use this valuable time to address any critical personal and legal matters. This includes advance medical directives describing how they want to be cared for as their disease progresses.
Steady Decline
The middle stages of dementia are the longest and most life-altering. Short-term memory continues to decline at a steady pace. People with dementia begin to forget more events in their lives, though more distant memories endure a bit longer. Days of the week, months, and seasons can become a fuzzy blur.
People need more assistance as ordinary daily life activities (dressing, bathing, toileting, eating) become more difficult for them. Driving is no longer an option, and people can no longer go on outings by themselves. Of course, this doesn’t stop many from wandering off, leading worried caregivers to call neighbors and police.
Faces of friends and family become more difficult to recognize. People with dementia become increasingly attached to the few people they remember (usually spouses). That is their remaining connection, one of the last few constants for them in what is turning into a strange, unfamiliar world.
Frustration, Agitation, and Paranoia
People in this stage become frustrated quickly. Their disease has advanced to such a point that interacting with people is a struggle. They still yearn to do so, but they have trouble following conversations and expressing themselves. This may show itself in mood changes.
Depression is common, and some become sad and withdrawn if they don’t have enough social interactions. Many get angry when they are confused. For example, when a caregiver tries to help with something that was once an ordinary, everyday, seemingly mindless activity like dressing or brushing their teeth. These stumbling blocks generate frequent sources of agitation. The most common crux comes in the evenings when people typically get ready for bed. Due to a phenomenon known as “sundowning,” evenings can be a time of worse frustration, confusion, and agitation.
It is scary for people with advancing dementia not to know where they are or who the people around them are. This can lead many to feel paranoid at times. Some even have delusions or hallucinations, thinking people nearby may be trying to harm them. People also lose the concept of what is appropriate: They may undress in public, make lewd or offensive remarks, or act in ways they would never have before. In other words, they lose their inhibition.
Final Stages
There is no sugarcoating it: The final stage of dementia is tough. People with dementia need round-the-clock care by then. They have trouble walking, sitting upright, and moving their arms or legs with purpose. They need someone to feed them and have progressive difficulty chewing and swallowing. Falls are a major hazard. They lose control over basic bodily functions like their bowels and bladder.
Communication is challenging. They can still speak but can’t carry on a conversation. Often, they will repeat a handful of familiar words, like an address, a date, a phone number, or a person’s name. As the final stage progresses, the last few words will fall by the wayside, and people will become nonverbal, aside from a few unintelligible sounds.
At this point, the most significant danger is not so much the disease itself but rather infections. People develop bedsores as they grow less mobile, and pneumonia is a frequent threat from aspiration (food or liquid getting into the airways) while eating and drinking. Because they cannot communicate, these problems might not get noticed and can become causes of death.
The end of dementia is extremely difficult. Family and friends have seen their loved one slowly slip away over many years. In the final stage, the disease may make them seem foreign and absent, but they are absolutely still alive. Those around them must make the most of rare moments of clarity. To the very end, people with dementia continue to benefit from having company and genuine human companionship. The desire for connection shines through the cloud of dementia, and having someone caring nearby helps give them peace.


 Learn
Learn Read Stories
Read Stories Get News
Get News Find Help
Find Help
 Share
Share
 Share
Share
 Share
Share
 Share
Share