Welcome to Psyched for Mental Health, the official mental health podcast of WebShrink.
In this episode, there is a poignant discussion about the biological, psychological, and social effect of the COVID pandemic with guest Dr. Jeffrey Barkin. In this first half of a two-part episode, we discuss the societal effects of the COVID pandemic, of catastrophes in general, long COVID’s effects on the brain, and more.
Episode Transcript:
The following is not intended to provide direct medical psychiatric or substance use treatment advice, and is not a substitute for evaluation and treatment by a healthcare professional.
Dr. Jeffrey Barkin:
And the scary thing is that long COVID seems to impact roughly one in five people with COVID. And now we just passed a million COVID deaths and probably it’s estimated half of America. So 175 million people have had COVID.
Dr. Edward Bilotti:
Hello, I’m Dr. Ed Bilotti. And this is Psyched for Mental Health, empowering you with trustworthy information about modern psychiatry. This podcast is a companion to webshrink.com. The platform for seekers and providers of mental health.
The COVID pandemic has been a life altering experience for all of us. The virus itself continues to be problematic. And as we continue to learn about variants and sub variants, it sometimes feels like this might never go away. Researchers continue to study the virus and are learning more about how it affects our bodies, including our brains.
What does it do to us once we have been infected? What is this phenomenon called long COVID? Are there psychiatric symptoms? The questions run deep. How do we, as humans, behave socially and psychologically in the face of a pandemic or catastrophic threats in general? Why did the 9/11 attacks bring us together, holding hands in the streets, literally, while COVID drove us apart?
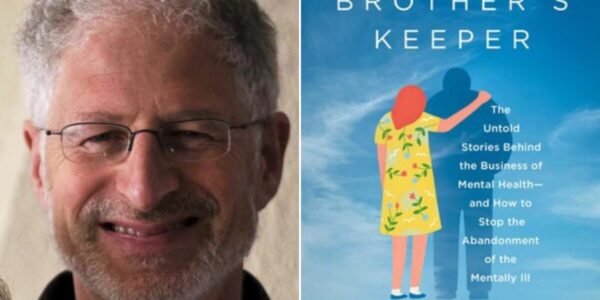
My guest, Dr. Jeffrey Barkin, is a Yale trained physician, board certified in general and geriatric psychiatry, a distinguished fellow of the American psychiatric association. He held a past academic appointment as assistant clinical professor of psychiatry at the University of Massachusetts Medical Center.
Currently he is associate chief medical officer of change healthcare. He practices both forensic and clinical psychiatry in Portland, and lectures nationally on healthcare policy analysis. Dr. Barkin cohosts a weekly radio show called “A Healthy Conversation with Steve Woods and Dr. Jeff Barkin,” which explores various perspectives and topics in healthcare.
He is also president of the Maine Medical Association. So let’s get started. Welcome Dr. Jeff Barkin. And thank you for joining me.
Dr. Jeffrey Barkin:
Thanks for having me. It’s great to be with you.
Dr. Edward Bilotti:
So we were planning to talk today about the mental health aspects of COVID, but in a broader sense, I guess we could look at it as mental health effects, catastrophes in general, and how that impacts mental health and then how we can look at COVID a little bit more closely.
Dr. Jeffrey Barkin:
That sounds good. We have sustained collectively a mass trauma over the past two and a half years, roughly by the time we’re recording this. Those of us who’ve been around long enough who live through 9/11 have really lived through two massive societal traumas.
There are probably few of your listeners that remember Pearl Harbor, but that is arguably another catastrophe that has happened on American soil, within American memory and imprinted in the DNA. Not that your listeners are limited solely to the United States, but in terms of trying to understand contemporaneous disasters, I think it’s helpful to think about perhaps things within our lifetime and things that we can relate to.
Dr. Edward Bilotti:
So what’s the difference between an external and an internal catastrophe? Can you help me understand that?
Dr. Jeffrey Barkin:
Sure. So catastrophe broadly speaking is what it sounds like it’s a mass event that has negative and deleterious impacts on a large number of people. And we’re seeing all sorts of catastrophes, whether they be war related in the case of the conflict and the Ukraine and Russia, whether they be climate related.
In the case of the weather, that’s sweeping, the United States, as we’re recording this. More and more people experience catastrophes, whether that’s the loss of life, illness, injury, loss of home or possessions. And certainly that’s what all catastrophes share in common is loss. That’s the common thread.
Those of us who’ve been around or mentioned in 2001 and 9/11 experienced a collective mass tragedy when the twin towers were struck by Al Qaeda using jets. And then the Pentagon was struck and we all experienced that. We saw that image over and over. It’s indelibly impressed upon all of our minds and brains.
We all experienced that trauma and we know what it was like. I, myself, through my family, lost several friends. So for those of us who had any connection to New York, it was deeply personal. And since we’re all connected, that was a catastrophe again, for those that can remember, that really touched all of us, but what was so amazing about that catastrophe was how it United us.
Remember how it united us.
Dr. Edward Bilotti:
Oh, absolutely. I remember like yesterday it seemed like immediately there was a palpable sense of unity among all of us. And that fear that there was an external sort of common enemy that could do this to us. And that, I, I don’t think anyone felt something like that could or would ever happen when it did.
And I was living in New Jersey at the time. And I remember my mother who lived in northern New Jersey in the house where I grew up from her back porch. You could see the plume of smoke coming up from the tower. So it was very close to home for me, but the unity was the most striking thing to me. And it’s hard for me to understand and even believe sometimes how things have come to be the way they are now with such divisiveness in our society when I remember that time, right after 9/11 right now.
Dr. Jeffrey Barkin:
External catastrophes are just like that. They are things that bring people together and lead to pro-social outcomes. So when 9/11 occurred, I was living with my family in Bangor, Maine, which is pretty rural. It’s a town of 32,000 people. And in small rural towns, you have your friends, you’ve got your neighbors who maybe you don’t like so much, the usual rivalries amongst the kids. But after 9/11, in our little city park, everybody came together, and I mean, everybody and we all held hands.
So that was the response to an external threat. It was an awful catastrophe, but it was prosocial in that all of the kids, all of the neighbors, all of those that hugged and had petty grievances or got together for dinner or excluded this one, we all were together. We all were collectively grieving. We all were holding hands.
Now, contrast that to COVID and pandemics. And in pandemics, we can’t come together and, and grieve together. We can’t hold hands. It’s dangerous and that causes a big, big difference in the way that people process infectious catastrophes. And if you think about this, historically, think about the approach to people with leprosy.
We isolated people with leprosy and created leper colonies. We isolated people with tuberculosis and put them into tuberculosis asylums. And more recently in Sub-Saharan Africa, when healthcare workers went to help out during the Ebola crisis, those healthcare workers were murdered, were slaughtered because people were afraid that their efforts would lead to reinfection, even though the folks were there to treat them.
So the response to infectious catastrophe is antisocial and rips people apart. We have to physically distance social distance and for a number of forces, which we could discuss. Cuz I think they’re, they’re amazing and fascinating psychosocial forces. The COVID pandemic has been a factor that’s ripped our society further apart than ever before.
Dr. Edward Bilotti:
Yeah, that is fascinating because, I have to say, I haven’t thought of it that way. My impression was that all of the political divisiveness and the tribalism and the left versus right, and social media, the way the social media algorithmsc, would feed people just that, which you know, which was consistent with the interests that they expressed.
And what you’re saying is really fascinating to me because I hadn’t thought of it that way, but it makes perfect sense.
Dr. Jeffrey Barkin:
During pandemics people’s primary fear is that they’ll be infected or that members of their family will be infected. And that sense of we will be infected by them. Us versus them becomes a root for tribalism and became exploited.
Now pre COVID, just to sort of go back a little bit and, and make it a little more personal. My last activity, my last social activity before COVID, before the March 15th lockdown, I was at a celebratory party. At a barbecue place of all places in Portland, Maine, and we were celebrating the win on vaccination, meaning that children in schools would continue to get their vaccinations.
If you remember back in, uh, 2020, issue number one was about, it was really an anti-vaccine issue and the thing was all anti pharma, but it was to increase the number of philosophical and religious exemptions for school children.
Dr. Edward Bilotti:
And we’re not talking about COVID vaccine here. We’re just talking about traditionally the vaccines that kids always got, even before we knew anything about COVID.
Dr. Jeffrey Barkin:
So these were MMR, Robella diptheria, typical DPT childhood vaccinations. And this became a very strong political issue. And the, the individuals that inhabit that political space before COVID really represented a very broad coalition of different stakeholders. On the one hand you had some right wing people who were really into personal freedom, who didn’t wanna have anything to do with mandates from schools or local governments.
On the other hand, you had people on the left that were very much into drug companies are bad and evil, and it’s a conspiracy and we have to do everything naturally. And then somewhere in the middle, you had a large number of folks who felt well, listen, vaccines work really well, but parents and patients should retain the right to decide what vaccines they get.
So before COVID, we lived in a climate that was very different than where we were before. So previously, and, and I may be somewhat older than you, but when Jonas Salk invented the polio vaccine, it was greeted not with any political outbursts, but by a ticker tape parade and a Nobel prize.
Dr. Edward Bilotti:
If I’m remembering the history correctly, he made it public domain, right. He kind of gave it away without seeking any personal profit or gain from it.
Dr. Jeffrey Barkin:
That’s correct. The Jonas Salk Institute was founded and it went from there. In fact, he was involved in a vicious, truly vicious in the good sense of vicious, like a good, uh, sports game match against his European rival.
And it was the first and best, and we eradicated polio and it brought the scientific and medical community together, real partying, real happiness, the opposite of what we’re seeing through COVID.
Dr. Edward Bilotti:
But it’s interesting though, the difference socially in that his mission was okay. I’ve discovered something that can really do something beneficial to mankind. And it’s important that I make it available. And it’s not about my personal profit, which stands in sharp contrast to modern corporate pharma.
Dr. Jeffrey Barkin:
That’s part of it. I think another big part of it. And I’ve studied this a fair amount. I obviously money is a big, big motive, but back when polio vaccine came out, media was much more monolithic, meaning that we had three networks, PBS and a couple independent stations.
So our set of facts were more shared. We tended to have a fairly authoritarian, typically white, elderly male behind a desk wearing a suit, delivering information. And we all heard the same thing. It was normative before that for families to gather around even the radio and share information. And we all had a set of shared facts, but in the 1980s, that changed.
The news formats changed with Good Morning America and the Today Show changing their set design actually to a living room set with a fireplace. So rather than having the objective distance of a desk, a piece of furniture with that physical boundary. Now the news is the living room and you’re there with the anchor in the intimacy of the living room with a fire roaring with more attractive anchors wearing makeup with men and women commingling often with a fairly flirtatious theme rather than a Walter Cronkite authoritative theme. So we saw this shift in media and then fairly soon thereafter, we saw the emergence of many, many more media outlets when cable became pre-eminent.
Upon the dawning of the internet, we saw the development of companies that were able to distribute content like Twitter or Facebook, but without the constraints, the legal constraints of broadcast. So for example, when we go on broadcast radio or TV, even though our program may be supported by advertisers, if we say something false and deceptive or use certain words, we are violating law and can be fined.
That’s not true on the internet. So the internet allows speech that is purely unregulated and what is further happened just to sort of bring us to the more present day is we have so many media outlets, competing for a fixed number of eyeballs and ears that in order to get listeners and viewers, you need to become increasingly outrageous so that in the selection of stories to cover.
We’ve developed sort of a rage industrial complex so that in order to court advertisers and get ratings, and this is all well documented, one has to actually have content that’s outrageous. And that has contributed, I believe, to the dissolution of shared facts absolutely.
Dr. Edward Bilotti:
It’s all perfectly logical to me.
You pointed out how the difference between 9/11 and COVID and one brought us together as a society holding hands and the other pushed us apart. Is that what you mean by an external versus internal catastrophe? I would’ve thought that COVID would also be an external catastrophes since it’s something that’s coming from nature outside of our control.
Dr. Jeffrey Barkin:
What I mean by an internal catastrophe is that it comes from us. So that in the case of COVID, one can have, COVID assuming one even believes that it exists, not know that you have COVID and at the beginning of the epidemic, infect other people for two weeks at a time and not even know it. So that’s a deep internal threat.
That’s not something as visual as airplanes flying into buildings or bombs landing on aircraft carriers destroying them. It’s an internal threat. That’s that’s spread internally from one person to another internally, not from an external threat and it makes it so that the internal threat is so life threatening, that it provokes an antisocial.
I don’t wanna hold your hand. Don’t get near me. We better physically distance rather than an external threat than 9/11, where we can mourn together, come together and safely literally hold hands.
Dr. Edward Bilotti:
Then you had this whole emergence of the deniers and the people resistant, you know, masks, uh, I don’t wanna wear a mask.
A mask is gonna, you know, make it harder for me to breathe, or this is a conspiracy they’re trying to shut us up by covering up our mouths or all kinds of ideas that began to flourish and propagate out there. And my feeling as a, a fellow psychiatrist was, this is a way of coping with fear.
Dr. Jeffrey Barkin:
Yeah. It’s absolutely a way of coping with fear, but what really got generated in addition to fear was rage.
And a term that gets thrown about in the tech world is engagement. And engagement loosely speaking is the number of times somebody clicks a link and how much time they spend on that link. So the most engaging content. From a psychiatric perspective is limbic system, in particularly amygdala oriented content.
That is to say, I realize that not everybody listening is gonna appreciate neuroanatomy, but maybe we could spend just a minute on how to get somebody’s attention. Right?
So the brain can loosely be organized into three brains where maybe the most primitive brain we might agree is the hypothalamus and regulates thirst and our blood pressure and sometimes anger, but fairly primitive things.
And the next level is our emotional brain. Our so-called limbic system makes us feel emotions. And a good part of the real estate of limbic system is an almond shaped region called the amygdala. And the amygdala makes us feel fear and anger.
And the third level of our brain is our frontal lobes. And that’s the part that helps us think that makes us think. So you have the lowest level, the sort of primitive brain, the hypothalamus, and then the mid-brain the limbic system and all that feeds to our conscious minds where we think, but it turns out that if you really wanna get somebody’s attention and derail them, grab that emotional mind.
And the best way to do that is to generate fear and rage. And that’s because fear keeps us alive. When we see something that’s threatening, our amygdala activates makes us fearful and respond to keep that thread away. Unfortunately, that may have been a really wonderful mechanism back a million years ago in the jungle.
But today that’s not a good mechanism when you’re responding to a post that you, you read on Twitter, for example, and it’s making you rageful and making you wanna attack and perhaps hunt somebody down who posted a tweet. So we’re seeing the same emotional response. To content. That’s not concord to that level of rage.
Dr. Edward Bilotti:
I mean, I completely understand what you’re saying about how to get someone’s attention and an environment where there is information overload and people have bombarded with, you know, a million choices of television shows and streaming and radio and podcasts like this one, uh, that it becomes harder and harder to get someone’s attention.
I think that’s why we saw this trend, not just in the, in the way the news is presented in the media from when you talked about the days of Walter Cronkite to, uh, today that also all of the, uh, entertainment content on, uh, television, and even on radio, you know, you have people like Howard Stern, you know, who basically made his whole career based on shock and getting attention and, uh, pushing the envelope. It’s hard to, to watch any television show these days without vulgar language, et cetera, because anything else at this point seems dry and dull and boring. Right?
Dr. Jeffrey Barkin:
And, and the other component is that throughout the country, there are news deserts.
So if you look at the number of counties without a newspaper, it’s going up. But one of the things that I like to ask people when they give me information is, oh, where’d you hear that? Where’d you read that? And I’m kind of used to answers probably like you are. Oh, I read that in the New England Journal of Medicine or American Journal of Psychiatry or the New York Times or the Wall Street Journal.
But now I hear no, I read that on Facebook, generally speaking. We’re not trained in how to vet and source the veracity of information in general, back in 1996, interestingly, the Federal Communications Commission changed the structure of things and news departments were able to report to the entertainment divisions and stations didn’t have as many ownership limitations imposed on them.
So it became more important for news to get ratings rather than put out news. That was under a Democratic president that was not under a Republican president. So these are really complicated social forces. But I think now we live in a country where a large number of people don’t have an anchor point for facts.
I think that we’re bombarded with information. I think the way that us doctors present information also could use a little bit of refinement. I do a radio show, a weekly radio show on a commercial station in Portland, Maine, and it’s available online anytime. And we have listeners all over the world. It’s called A Healthy Conversation and it airs on the conservative station because it reaches an audience that otherwise would not have access to the sort of facts I try to provide, but in a calm way.
I also think that us doctors aren’t necessarily trained to talk to people who may not be doctors. And I like to remind myself that when somebody sees me for the first time, that may be the first time that they’re interacting with a psychiatrist. And I will remind you and your listeners that, generally speaking, when you’re talking to a doctor or a lawyer or a professional.
We’re not always the ones giving you the best news. We’re not serving you birthday cake and delicious pizza. We’re usually giving you bad news. So I remind myself that, you know, we’re ambassadors and emissaries, so we have to kind of clean up our act and how we communicate.
And I think part of that is sharing our own humility and uncertainty over facts to allow it so that people can allow our information to evolve without later accusing us of being deceptive or being liars. When in fact we didn’t never lied. It’s just that the fact pattern changed. So if you think about COVID early guidance from the CDC was to not wear masks.
Well, we later learned that this is an aerosolized, highly transmissible respiratory disorder. So it’s very easy to say, well, you lied to me about the masks. Well, no, at the time people really thought that this was a surface contact disease and people were cleaning their grocery bags. So what we, what we knew then is different than what we know now, but a lot of people misinterpreted that as purposeful lying when in fact it was just the evolution of the knowledge. Right.
Dr. Edward Bilotti:
I remember at the time there was all sorts of emphasis on the news networks about how to wash your hands correctly and how to clean surfaces.
Dr. Jeffrey Barkin:
Well, I could tell you what I do and, and that is, I always wear a mask if I’m in a high population area.
So if I go to the supermarket, the drug store, uh, I actually saw my first movie. For the first time in two and a half years, I saw Top Gun: Maverick and I wore my N 95 mask with my Maine Medical Association mask over that. So I was double masked it was a great movie worth seeing.
Dr. Edward Bilotti:
Yeah. I’ve uh, I’ve heard about it. I have a cousin who lives out in the Los Angeles area, who is a pilot and his name is Kevin LaRosa and he actually flew the planes and, uh, helicopters for a lot of the scenes in that, in that movie. So, uh, I have not seen it yet, but. Thanks for the tip. I’m, I’m definitely going to plan to see it and I’ll wanna see it on a big screen. And I will wear a mask.
Dr. Jeffrey Barkin:
In my experience, most people don’t want to be told what to do. They instead want to ask you, what do you think I should do? Or they wanna know, well, what would you do? So I’ve begun as a communicator rather than tell people what to do. I share what I do. And often they’ll say, well, why, but I’ve been able to get a lot more people on board and vaccinated and wearing masks and make this not a political or silo dialogue, but rather a healthy conversation, which is quite literally the title of the show.
Dr. Edward Bilotti:
It follows the basic underlying principles of motivational interviewing, which is something that we use a lot in, uh, substance use, which is, you know, not, I’m not gonna tell you what to do. I’m not gonna judge what you choose to do, but I’m gonna help you understand why you’re choosing to do things the way you’re choosing to do things and understand your own ambivalence and provide support and, and information and education where I.
That might be of help to you. And in fact, that’s actually one of the [00:25:00] goals and missions of this podcast and of web shrink.com is to make medical information more accessible to people in a, in a much more, um, approachable, accessible, safe way that they can search and find the answers that they’re looking for.
So having said all that, let’s talk about the mental health aspects specifically of COVID. So COVID had the effect on our society of. Pushing us apart, but on a more individual level within, for an individual or for a family, how would you say COVID has impacted mental health?
Dr. Jeffrey Barkin:
Well, the first part is how hasn’t it?
So maybe, maybe by starting there, we can kind of go back to a model that may sound somewhat anachronistic, but the biopsychosocial model. And I think we sort of started with the social piece discussing internal versus external catastrophes and the impact on society, the divisive impact, I would say before we go to the biologic and psychologic.
We gotta talk about that is that us doctors have to remember that when people don’t wanna wear masks and that they’re against mandates and they’re not physicians and they’re not scientists. We have to put on our empathy hats, not our, not our anger, hats. And we have to do a good job, a much better job than we’ve done well asking. Well, why, why would people be against a shutdown?
Why would anybody wanna be against shutting things down when people are getting sick? Well, a lot of people were opposed to the shutdowns because it was shutting down those businesses. And for those of us that are fortunate, that can work remotely. We were impacted much, much less, but for a lot of folks that are direct workers and can’t work remotely are overrepresented in demographics that don’t wear masks and that are not vaccinated. We know that in demographics where you have a larger number of one party over another, you actually do have excess death rates. I mean, that’s just a fact. So that’s an example of further example of how people who have certain risk.
And I would say a lot of that is, is poverty where you have people who are laborers, who are exposed to the public, who can’t go remote. And in order to economically support themselves they can’t be shut down. And I think that that was another root cause that stoked the anger and that combined with politics and social media to lead to the ridiculous number of deaths.
So maybe that’s a natural transition into the biology of COVID the biopsychosocial model for those joining is just a model that, you know, when, when Dr. Bilotti or I see a patient. Everybody’s so complicated. How can we begin to understand? And it’s first, what’s the biology of the person’s presentation and what’s the psychology. And then what’s the social context of this. And I think we did a good job of discussing the social context. Maybe we could talk about the biologic.
Dr. Edward Bilotti:
Absolutely. Yeah. And in our premier episode of psych for mental health, Dr. Allison Malloy did an excellent job of explaining how difficult psychiatrists work is for that very reason, because we don’t just wanna know what’s your symptom, uh, you know what bacteria is causing this infection and here’s this antibiotic that’s gonna treat it.
We wanna know about the whole person. We wanna know what’s going on psychologically for you. What’s going on medically. What’s going on, family history. What’s going on socially. And absolutely it’s um, it’s not easy work but sure.
Let’s talk about the biology of COVID.
Dr. Jeffrey Barkin:
So the biologic part of COVID itself could probably require countless episodes. It’s so fascinating, but what we’re learning now is that SARS COVID 19 and its various variants and its lineage groups, including Omicron and the subomicron lineages are really active at inducing an immune response that is vascular. So you see this playing out at the end organ level at the small vessel stage, why some people get impacted and other people don’t is unknown. And there’s a large amount of research trying to figure out, you know, are there biomarkers?
So I know of some groups that are doing some machine learning of taking large copious medical records and data, mining them to see what attributes make it so somebody who is infected get sick or maybe even gets infected in the first place or what is it about people that don’t get COVID or get infected, but don’t get sick and what’s becoming increasingly clear is that there are some biomarkers. It’s being refined, but that these biomarkers lead to inflammation and an inflammatory response at the end organ and in the brain.
That’s really kind of like our organ of concern in psychiatrists, because it begins to be the case that the immune system, the cytokine response to the immune response against COVID in the itsy bitsy, teeny weeny parts of the brain are causing the lesions. That’s the sort of compelling thinking now of long COVID from a biologic perspective, as well as myocarditis and some of the inflammatory features involved now, what is it about people that develop long COVID.
That’s an area of ongoing inquiry, but the psychiatric components are profound and look a lot like though separate from traumatic brain injury, which also in the final analysis is a microvascular like presentation where you have diffuse, neuronal, distributed deficits. It’s not like a stroke where you have a fixed lesion. And it’s just that lesion rather lesions of long COVID like traumatic brain injury tend to be much more all encompassing. So things like decreased attention, decreased processing speed, certainly fatigue. So people who develop various infectious diseases that impact the brain can develop chronic fatigue syndrome.
And certainly that’s the case with COVID. I, I have a coworker right now who’s an infectious disease doctor who just got COVID herself and she’s exhausted. Absolutely just exhausted falls asleep for a minute and four hours goes by. So it’s clear that there is a profound effect on the central nervous system.
The other systems that get affected when people get long COVID, so-called long COVID are the cardiovascular system and people will feel exhaustion and they’ll feel incredible lack of physical stamina. So a patient of mine who is a marathon runner gets out of breath and tachycardic walking up just a few steps, not a flight of steps, just a few steps.
So it’s this concept of dysregulation, both at the cardiovascular level and certainly at the central nervous system level that seems to be relevant to what’s causing this thing we call long COVID. And the scary thing is that long COVID seems to impact roughly one in five people with COVID and now we just passed a million COVID deaths and probably it’s estimated half of America, so 175 million, people have had COVID.
So now that we have the dominant strain, as we’re recording this as Omicron, which is incredibly infectious, There is now data that suggests that even patients that don’t have severe disease, a good percentage of those can go on to develop long COVID. So the effects on workforce, workforce shortages, that we’re seeing more and more of are really quite profound.
And that results from the biologic effects of COVID, which is this profound, terrible exhaustion. Now, a lot of people will get respiratory symptoms like cough, shortness of breath, congestion, headache, and those symptoms. But the one that really disables folks is the fatigue, the brain fog, the, I have no energy.
And there are patients in the definition of long fatigue varies. There are different definitions, but basically I sort of think of anything that goes on more than three or six months is long COVID and I’ve now seen several cases of long COVID. And what’s clear to me is that we have very little research to guide the treatment of long COVID.
Dr. Edward Bilotti:
It’s interesting. You talk about lesions in traumatic brain injury. There, there can be gross lesions that can be visible on, on scanning and imaging, MRI, and CT scan. And then there can be functional deficits that there is no grossly visible lesion or abnormality that we can see, but there are functional impairments resulting from the, uh, traumatic brain injury. So when you say lesions, do you mean actual lesions? That can be visualized.
Dr. Jeffrey Barkin:
Well, in the case of COVID no, not yet. In the case of traumatic brain injury, you have a large amount of research showing that repeated head injury can cause chronic traumatic encephalopathy, which is diagnosable at autopsy. We don’t have that data with COVID brains yet.
I have spoken with pathologists who have all shared with me that this is inflammatory and that patients have elevated levels of cytokines and cytokine releasing factors, which cause an a localized, inflammatory response. And that’s thought to be the basis of the myocarditis that some patients get an association with both some vaccines, but also with COVID itself.
And it’s thought that that kind of response is the case in the brain as well, because these. Inflammatory processes can occur beyond the blood brain barrier. So it’s not like the blood brain barrier protects you. So in order for the brain to be healthy, it has to have bodies and other mechanisms to keep viruses and, and things from attacking brain cells.
So it’s thought that the immune system fighting back on the COVID may be the thing that’s relevant in treating long COVID. And, and again, what would support that, that some of the disease modifying. Drugs that lessen the immune response also have been very helpful in some patients such as steroids, methotrexate, some of the disease modifying drugs like Humira, Cosentix, Embrel and Taltz have also had, again, all of this is off FDA label, but they’re anti-inflammatory treatments.
So there’s some emerging thinking and hope that by dampening down the immune system, we’ll be able to have some approaches to long COVID.
Dr. Edward Bilotti:
So the lesions quote unquote, in the brain from these inflammatory responses resemble, the effects of those lesions resemble those of a traumatic brain injury presenting with brain fog and concentration difficulties, some impaired, um, executive function, perhaps, and fatigue.
What about psychologically?
Dr. Jeffrey Barkin:
Boy. I’m so glad you brought that up. So we talked a little bit about the sociology and a little bit just now about the biology, but the psychology is profound.
Dr. Edward Bilotti:
This concludes part one of my conversation with Dr. Jeffrey Barkin in part two, we will continue with more about the psychological impacts of COVID the role of physicians in the media.
We all remember the TV doctors who were front and center during the worst parts of it. And Dr. Barkin will give us his special prescription for coping with stress and avoiding burnout you won’t wanna miss.
Thank you for listening. This podcast is a companion to web shrink.com. Visit webshrink.com where you’ll find original, trustworthy, and authoritative content to help you find the answers you need about mental health and addiction, mental health professionals, and facilities.
List yourself in WebShrink’s provider directory. Go to webshrink.com and click list to your practice.
The Psyched for Mental Health podcast was written and produced by Dr. Ed Bilotti, co-production and sound editing by Nathan Tower and Aaron Devo at Nonsensible Productions in Portland, Maine.

 Learn
Learn Read Stories
Read Stories Get News
Get News Find Help
Find Help
 Share
Share
 Share
Share
 Share
Share
 Share
Share